The 4 Stages of Congestive Heart Failure: What You Need to Know
OCTOBER 03, 2022
By THE CORMEUM TEAM
Congestive heart failure (CHF) “is a condition in which the heart cannot pump enough blood to meet the body’s needs, or can do so only at abnormally high filling pressure.”
About five million people in the U.S. are living with CHF, and about 550,000 new cases are diagnosed each year.
Left untreated, CHF can lead to death. However, there are ways to manage the condition, extend your life and even thrive with heart failure. The first step is understanding what heart failure is and how to manage it.
Keep reading to learn how heart failure is classified, common symptoms and what to do after a heart failure diagnosis.
Stages and Classes of Heart Failure
There are two widely accepted ways to place a patient along the continuum of heart failure severity: subjective and objective. Both are divided into four groups, and both can be useful when patients and their providers discuss treatment options.
- Subjective classification. The New York Heart Association (NYHA)’s heart failure classification is based on the severity of symptoms reported by patients.
- Objective classification. The American Heart Association (AHA) and American College of Cardiology (ACC) have identified four stages of heart failure more heavily based on diagnostic criteria.
Four Stages of Heart Failure
The AHA/ACC’s stages help patients understand the progressive nature of heart failure, and give patients and providers a clear way to discuss the disease.
Stage A: Pre-Heart Failure
Patients in this stage are at high risk of developing heart failure. They likely are not experiencing symptoms but have one or more of the following conditions:
- Hypertension
- Coronary artery disease
- Diabetes
- Metabolic syndrome
- Family history of cardiomyopathy
- History of rheumatic fever
- History of alcohol abuse
- History of taking drugs that can damage the heart muscle, such as some cancer drugs
Stage A heart-failure patients will work with their providers to implement lifestyle and pharmacological interventions including:
- Smoking cessation
- Treating hypertension
- Regular exercise
- Control metabolic syndrome
- ACE inhibitors or ARB medications as appropriate
Stage B: Silent Heart Failure
Patients in Stage B heart failure have not experienced symptoms of heart failure, but they have diagnosed structural damage to the heart. Stage B heart-failure patients may have:
- Suffered a previous heart attack
- Had an echocardiogram that shows an ejection fraction (EF) of 40% or less
- Experienced asymptomatic valvular disease
The AHA recommends patients in Stage B follow the therapy goals laid out in Stage A, and add appropriate prescription medications in consultation with their provider.
Stage C: Symptomatic Heart Failure
In stage C, patients have structural heart disease and are experiencing symptoms of heart failure. The most common congestive heart failure symptoms are:
- Shortness of breath
- Fatigue
- Reduced ability to exercise
- Swelling of the feet, legs or abdomen
It’s critical for patients in Stage C to limit salt intake, as too much salt in the diet can cause fluid to build up around the heart. Patients should continue to practice measures laid out in previous stages. Providers may also:
- Add ACE inhibitors, beta blockers and/or diuretics
- Monitor weight
- Restrict fluids
- Recommend devices such as biventricular pacing or implantable defibrillators
Stage D: End-Stage Heart Failure
Patients in Stage D have significant symptoms that do not get better with treatment. Often they are hospitalized and cannot be discharged without specialized interventions. Stage D heart-failure patients experience symptoms even when they are at rest or with minimal exertion.
In Stage D, patients will continue to work with providers to decide on the best level of care. According to AHA, options include:
- Compassionate end-of-life care (hospice)
- Extraordinary measures like heart transplant, chronic inotropes or permanent mechanical support
- Experimental surgery or drugs
Four Classes of Heart Failure
While the AHA and ACA have organized heart failure into stages A through D that takes into account diagnoses and symptoms, the NYHA has laid out a functional classification system that categorizes patients based on limitations during physical activity. The four classes are:
Class I: No limitation of physical activity
Class II: Slight limitation of physical activity
Class III: Marked limitation of physical activity
Class IV: Symptoms occur even at rest; discomfort with any physical activity
Stages and Classes: Side by Side
The chart below, created by Heart-Failure.net, shows how the stages and classes align. Both classification systems offer patients and their providers information about how to treat and manage heart failure.
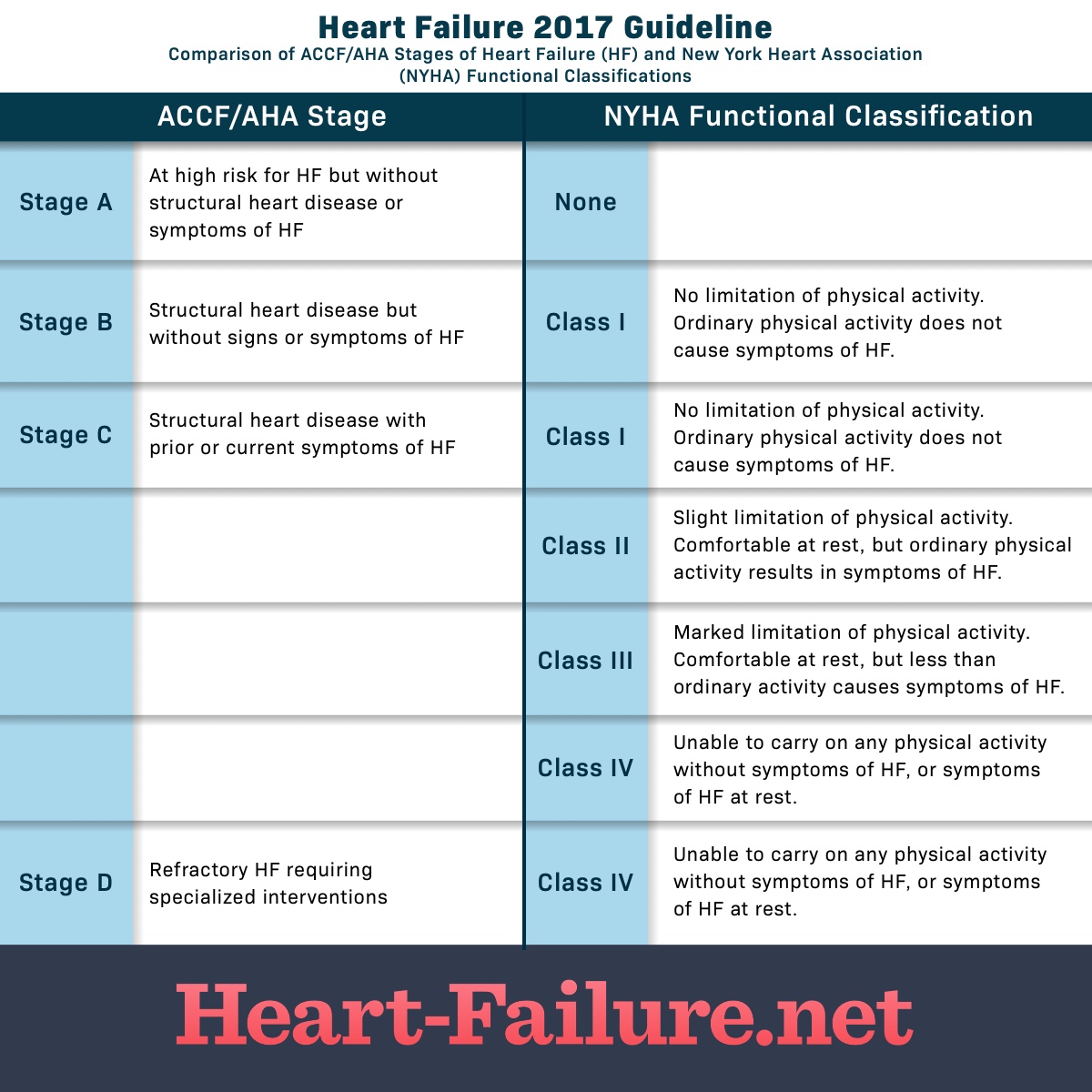
Source: www.heart-failure.net
Living With Heart Failure
Heart failure is a continuum, and managing it day-to-day takes dedication from patients and providers. To avoid progressing to the next stage, patients should keep in compliance with all prescribed medications, follow a heart-failure friendly diet and have regular checkups with providers.
Research has shown that patients who play an active role in their treatment tend to have better outcomes. Take control by implementing the following changes and routines into your daily life:
- Change your diet. Under the supervision of your provider, implement a low-salt diet. They may also recommend changes to your fluid intake.
- Monitor your health. It’s important to keep track of changes in your body like weight fluctuation, fluid intake and output, swelling or fatigue. It’s also crucial to know your vital stats, including blood pressure and weight.
- Stay positive. It can be hard to have a positive attitude, but stress, anxiety and depression can exacerbate your symptoms. Stay connected with family and friends, find a support group, meet with a therapist and continue to practice hobbies you enjoy.
- Ask questions. Your provider is your teammate as you navigate living with heart failure. Make sure to share all data you’ve gathered between visits and ask any questions you might have.
Heart failure is not curable, but new treatments are being developed every day to help patients live and thrive with heart failure. Technology — in the form of smartphone apps — has also made it easier for patients to track and monitor everything from symptoms to salt intake and share with their providers.

