Signs of Worsening Heart Failure and What to Do About It
OCTOBER 04, 2023
By THE CORMEUM TEAM
As you adjust to living with heart failure, you’ll begin to see patterns emerge in how the disease affects how you feel, both physically and emotionally. You may notice not just the ebb and flow of your symptoms but also certain health metrics that play a pivotal role in understanding your disease. Some days may be good where you don’t experience symptoms at all. On other days, you may feel too tired to get out of bed.
Regularly monitoring key health metrics such as sudden weight changes, fluctuations in blood pressure, and variations in heart rate can provide valuable insights into your condition. These metrics, combined with day-to-day symptoms like swelling or shortness of breath, paint a comprehensive picture of heart health.
Heart failure is considered a progressive condition. This means that over time, your heart’s ability to pump blood efficiently can deteriorate, leading to worsening symptoms and possible complications. How can you tell your bad day is just that — or an actual worsening of your condition?
In this article, we’ll unpack signs of worsening heart failure, offer guidance on self-management and tracking, and highlight which new or worsening symptoms warrant a call to your provider.
Knowing these signs can empower you to act when necessary and continue to effectively manage your condition as you learn to live well with heart failure.
Understanding Heart Failure: A Quick Recap
Heart failure is a condition in which the heart cannot pump enough blood to meet the body’s needs. It’s a common condition, affecting about 6.2 million adults in the United States.
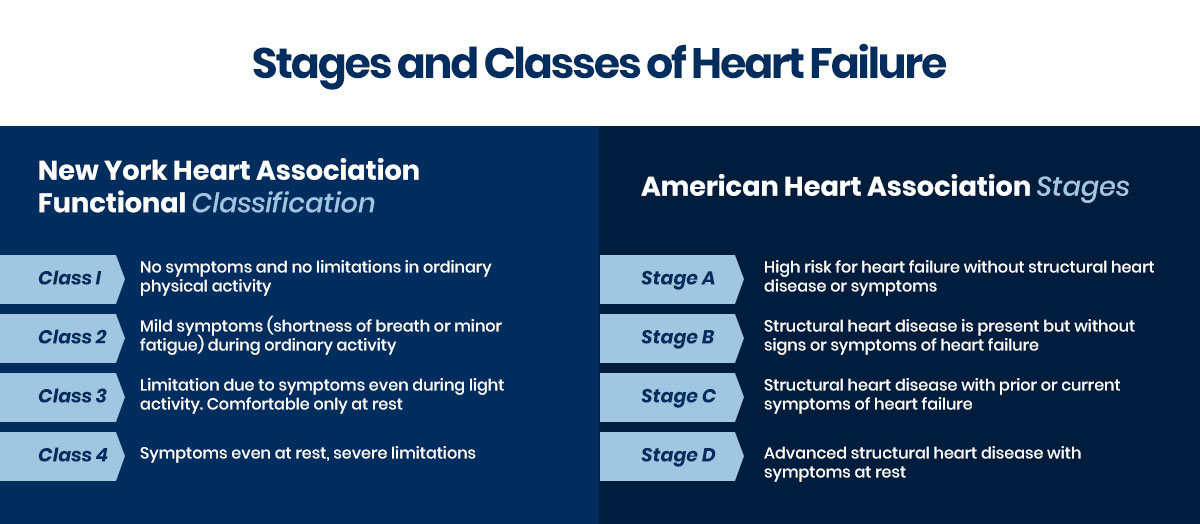
To understand the severity and progression of heart failure, medical professionals categorize it into stages or classes, which can help your care team tailor a treatment plan to your needs.
Signs and Symptoms of Worsening Heart Failure
Heart failure, while a common condition, is still fairly unpredictable. That’s because everything from symptoms to the progression of the disease varies greatly from person to person. You may go months or even years with few or no symptoms. Then, you may notice that activities that were once effortless, like climbing a flight of stairs, suddenly leave you breathless.
That’s why it’s so important to track and monitor your experience with heart failure. By keeping a close eye on the subtle changes in your body and how you feel, you can better communicate with your provider, ensuring your treatment plan is tailored to the current state of your heart failure.
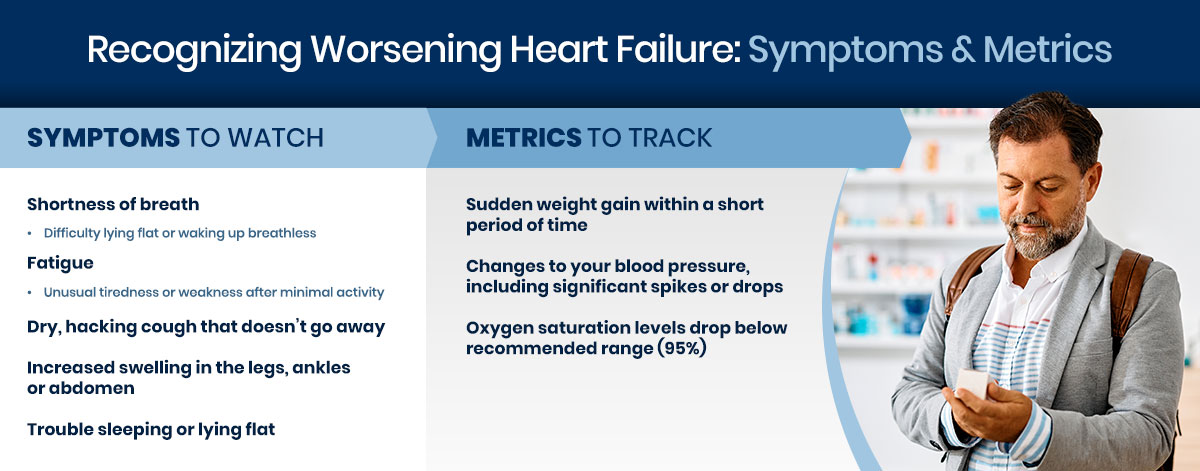
Day-to-Day Symptoms to Monitor
Your everyday experience offers clues to how heart failure is affecting your body. Check in with yourself often and track your symptoms and moods using a digital app like Cormeum. Some of the most common symptoms include:
- Shortness of breath. Notice whether you have trouble catching your breath. Do you find yourself gasping while exercising but breathing normally throughout the day? Or, is it hard to catch your breath while doing daily activities or even lying down?
- Fatigue or weakness. Pay attention to your energy levels. Do you feel drained even after a night’s rest or while performing daily tasks?
- Persistent cough or wheezing. How long has that cough been sticking around? A persistent cough can indicate fluid in your lungs.
- Swelling. Check for unusual puffiness, especially in the feet, ankles and abdomen. Maybe your clothes are fitting a little tighter around the middle. That could be a sign of fluid retention.
- Sleep issues. Do you have trouble sleeping or find it difficult to lie flat on your back?
The above symptoms are all commonly associated with heart failure, but they may not all be typical for you. If you start experiencing new-to-you or worsening symptoms, it’s important to make an appointment with your provider right away.
Important Metrics to Track
You needn’t rely only on what you feel when tracking the progression of your heart failure. Specific health metrics offer data that can be useful in understanding how your body is reacting to treatment and lifestyle changes. Track these alongside your symptoms for a clearer picture of your condition:
- Weight. The scale is tricky. It can fluctuate from day to day, but if you see sudden spikes, like two to three pounds overnight or five pounds in a week, check in with your doctor.
- Blood pressure. Knowing your blood pressure is good practice for those living with heart failure, as significant deviations from your normal can be cause for concern.
- Oxygen saturation. A drop in oxygen saturation levels below the typical range can suggest your body isn’t getting the oxygen it needs.
Depending on your care plan, your provider may recommend you track these metrics at home between visits. In addition to your bathroom scale, there are blood pressure monitors and pulse oximeters designed for home use. Talk with your doctor about when and how to use these aids, and be sure to track your readings regularly.
Heart Failure Self-Management
Knowing your baseline — what’s normal for you — is an essential first step. Effective self-management is just as important when it comes to living and thriving with a heart failure diagnosis. Heart failure patients who use self-management tools like mobile apps after a hospitalization are less likely to be readmitted.
Monitor daily. Keep a daily log of your symptoms and important metrics like weight, diet and fluid intake. This can be as simple as a notebook, but the digital age has given patients an easier way to track. The Cormeum app is designed for heart failure patients to track the metrics that are most important to them and their doctors.
Eat a heart-healthy diet. Your diet is important to maintaining health as long as possible with heart failure. This means reducing sodium and cutting down on saturated fats and added sugars. Many newly diagnosed heart failure patients find this the most challenging among recommended lifestyle changes — but changing your diet does not mean eliminating the flavors you love. Seek out chef-created recipes that offer all the flavor with none of the guilt.
Take your meds. This one seems like a no-brainer. Taking your medications as prescribed is critical. But taking the right meds at the right time and keeping track of whether you’ve done so can be challenging. Use an app to keep track of your medications, and share adherence with your provider.
Get active. Your health care team will give you specific guidelines on the type and intensity of exercise that you should be engaging in based on your current level of health. The key is to get some movement in each day.
Stay informed. Heart failure is a dynamic condition. Your experience with it may not be just like everyone else’s, but you can learn from what is typical and from best practices in treatments. Understanding your disease can empower you to make informed decisions and communicate effectively with your provider.
You’re Not In This Alone
As we mentioned above, heart failure is a progressive condition. Self-management can significantly slow the progression, but chances are your disease will worsen over time. When you notice new or worsening symptoms, it’s crucial to relay them to your provider right away.
The more open you can be with information — whether you detect worsening fatigue, a faster heart rate or new swelling — the easier it will be for your team to react proactively in adjusting your care plan.
Sharing data with your provider is one of the best ways to lean into that team mentality. When you’re able to provide an accurate account of the changes you’ve made and the metrics you’ve tracked between visits, your provider can craft the most effective care plan for you going forward. This can mean timely interventions, better management strategies and a more tailored approach to your unique experience with heart failure.
Living with heart failure can be overwhelming. There’s a lot to learn, track and monitor. But it’s important to remember that you’re not in it alone. Your health care team, your family, and your community are all committed to helping you manage your condition and live your best possible life in spite of a heart failure diagnosis.